If you’re wondering about getting top 50 HCFA code errors and resolutions for free, particularly related to HCFA forms, then you are at the right place. The HCFA form, or CMS-1500, is crucial in healthcare billing, standardizing the claims process for practices. However, errors can lead to costly delays and even claim denials. This guide outlines the top 50 HCFA code errors and their solutions, tailored for healthcare providers, billing experts, and anyone involved in medical billing.
Access additional 50 HCFA code errors and resolutions from the bottom of this blog for free
What is the HCFA Form?
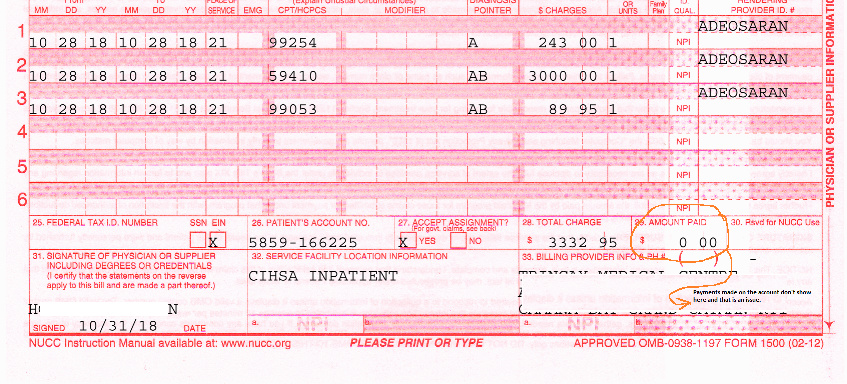
The HCFA, officially known as the CMS-1500 form, is a standardized medical claim form used to bill services for Medicare and private insurances. It plays a vital role in ensuring that claims are correctly filed, processed, and reimbursed.
Top 50 HCFA Code Errors and How to Resolve Them
1. Incomplete Patient Information
Error: Missing patient details like name, address, or insurance ID.
Resolution: Double-check entries or use EMR (Electronic Medical Records) software to autofill patient data accurately.
2. Incorrect Diagnosis Code (ICD-10)
Error: Using unspecified or incorrect diagnosis codes, such as F43.
Resolution: Use specific ICD-10 codes and stay updated with coding guidelines to avoid generic entries.
3. Outdated HCFA Form Version
Error: Filing claims using outdated CMS-1500 forms.
Resolution: Ensure the latest form version is always used.
4. Incorrect Procedure Codes (CPT)
Error: Using outdated or incorrect CPT codes.
Resolution: Carefully read CPT code descriptions and verify with coding manuals or billing software.
5. Missing Provider NPI Number
Error: Forgetting to include the National Provider Identifier (NPI).
Resolution: Always enter the NPI to avoid rejections or delays.
6. Invalid Dates of Service
Error: Incorrect dates or ranges in the service fields.
Resolution: Double-check service dates to ensure accuracy before submission.
7. Missing Patient Signature
Error: Omitting the patient’s signature on necessary forms.
Resolution: Verify that the patient’s authorization signature is present.
8. Incorrect Patient Relationship Code
Error: Wrong code for the patient’s relationship to the insured.
Resolution: Verify the correct relationship code to avoid claim processing issues.
9. Missing or Incorrect Modifiers
Error: Omitting or using inaccurate CPT modifiers.
Resolution: Apply specific modifiers relevant to the service provided.
10. Duplicate Billing
Error: Billing for the same service more than once.
Resolution: Ensure that each service is billed only once by reviewing claims before submission.
11. Unbundling Codes
Error: Billing separate codes for procedures that should be bundled.
Resolution: Use the correct bundled code to avoid inflating costs and penalties.
12. Incorrect Place of Service Code
Error: Selecting the wrong place of service code.
Resolution: Use a coding guide to ensure the place of service matches the location.
13. Incorrect Claim Filing Indicator
Error: Using an incorrect claim filing indicator.
Resolution: Check the appropriate claim filing indicator to ensure accurate processing.
14. Invalid Patient Gender Code
Error: Incorrect patient gender entry.
Resolution: Confirm the gender information with patient records.
15. Missing Service Facility Location Information
Error: Not including the facility where services were performed.
Resolution: Enter the service facility location accurately.
16. Incorrect or Missing Prior Authorization
Error: Not obtaining prior authorization for certain services.
Resolution: Confirm authorization requirements with insurers before performing services.
17. Outdated Fee Schedules
Error: Using old fee schedules that don’t reflect current costs.
Resolution: Update fee schedules regularly to ensure accurate billing.
18. Incorrect Rendering Provider Information
Error: Missing or incorrect rendering provider information.
Resolution: Enter the accurate details for each service provider.
19. Invalid Patient ID Number
Error: Using incorrect patient insurance ID numbers.
Resolution: Verify ID numbers against insurance documentation.
20. Incorrect Date of Birth
Error: Patient’s date of birth entered incorrectly.
Resolution: Confirm the date of birth matches patient records.
21. Missing Patient Account Number
Error: Not including the patient account number.
Resolution: Ensure this number is recorded on all submissions.
22. Incorrect Referral Information
Error: Missing or incorrect referring provider details.
Resolution: Always verify referral details before claim submission.
23. Missing Tax ID Number
Error: Omitting the provider’s Tax ID number.
Resolution: Double-check that Tax ID information is present on the form.
24. Invalid Diagnosis Pointer
Error: Using the wrong diagnosis pointer for CPT codes.
Resolution: Ensure the diagnosis pointer correctly references the ICD-10 code.
25. Incorrect Payment Assignment Indicator
Error: Choosing an incorrect payment assignment indicator.
Resolution: Confirm the assignment indicator to align with payer guidelines.
26. Missing Emergency Indicator
Error: Not marking emergency services as such.
Resolution: Mark emergency services accurately when necessary.
27. Invalid Patient Status Code
Error: Incorrect patient status (inpatient, outpatient).
Resolution: Confirm and enter the accurate patient status code.
28. Incorrectly Marking Resubmitted Claims
Error: Not marking claims correctly as resubmitted.
Resolution: Use the appropriate resubmission codes to avoid duplicate denials.
29. Invalid Procedure Code Quantity
Error: Incorrect quantity on CPT or HCPCS codes.
Resolution: Ensure the quantity reflects services performed.
30. Missing Reason for Visit Code
Error: Not including the primary reason for the visit.
Resolution: Verify the reason for visit matches diagnosis codes.
31. Incorrect Coordination of Benefits
Error: Misrepresenting or not including primary/secondary payer info.
Resolution: Confirm coordination of benefits with payers.
32. Missing or Incorrect Deductible Details
Error: Failing to account for patient deductible amounts.
Resolution: Ensure deductibles are calculated and applied correctly.
33. Failure to Note Additional Procedures
Error: Not coding multiple procedures when applicable.
Resolution: Use codes for each additional procedure.
34. Incorrect or Missing Resubmission Codes
Error: Leaving out resubmission codes for corrected claims.
Resolution: Include resubmission codes for each correction.
35. Missing Supervising Physician Details
Error: Not including required supervising provider details.
Resolution: Enter supervising provider details if necessary.
36. Unspecified ICD-10 Diagnosis Code
Error: Using broad ICD-10 codes.
Resolution: Use the most specific ICD-10 code for each diagnosis.
37. Incorrectly Billed Global Period Services
Error: Billing for services within a post-operative global period.
Resolution: Verify global periods to avoid duplicative charges.
38. Missing Medical Necessity Documentation
Error: Lacking documents to justify medical necessity.
Resolution: Ensure all medical necessity documents accompany the claim.
39. Incorrectly Entered Units of Service
Error: Incorrectly billing service units.
Resolution: Enter the correct service units.
40. Incorrect Provider’s Service Start Date
Error: Mistakes in service start dates for providers.
Resolution: Confirm and enter accurate start dates.
41. Misalignment with Payer Guidelines
Error: Failing to follow payer-specific coding rules.
Resolution: Stay updated with each payer’s unique billing rules.
42. Failure to Sign Form CMS-1500
Error: Leaving required fields unsigned.
Resolution: Confirm all required signatures are present.
43. Incomplete Itemized Charges
Error: Not providing full itemization of charges.
Resolution: Include all itemized charges on the form.
44. Incorrect Care Setting Designation
Error: Mislabeling care setting (e.g., inpatient, outpatient).
Resolution: Ensure accurate entry of care settings for all claims.
45. Missing Contact Information for Patient
Error: Omitting patient contact details.
Resolution: Verify and complete contact information fields.
46. Failure to Note Insurance Coverage Type
Error: Leaving out primary/secondary insurance type.
Resolution: Indicate the insurance type for each claim.
47. Invalid Principal Diagnosis
Error: Using an incorrect principal diagnosis code.
Resolution: Choose a principal diagnosis accurately reflecting the primary condition.
48. Incorrectly Assigned Claim Amounts
Error: Entering wrong claim amounts.
Resolution: Double-check claim amounts for accuracy.
49. Missing Signatures on Claims Adjustments
Error: Missing required adjustments’ signatures.
Resolution: Confirm all claims adjustments are signed.
50. Timeliness of Filing Claims
Error: Filing claims after payer deadlines.
Resolution: Submit all claims within 30 days of service whenever possible.
Tips for Avoiding Common HCFA Errors

Invest in EMR Software
- Streamlines Data Entry: Electronic Medical Record (EMR) software helps automate much of the data entry process, minimizing manual input errors. It ensures that information like patient demographics, insurance details, and service dates are accurately transferred onto the HCFA forms.
- Reduces Coding Errors: Many EMR systems have built-in coding features that suggest the most accurate CPT, ICD-10, and HCPCS codes, reducing the chances of using outdated or incorrect codes.
- Facilitates Compliance: EMR software often includes alerts and reminders for compliance updates. This can help keep your practice in line with constantly changing coding standards, fee schedules, and payer guidelines, which is critical to avoid rejections.
- Improves Accessibility and Record Keeping: An EMR system centralizes patient records, making it easier to retrieve necessary documentation for claims, appeals, or audits, thus enhancing accuracy and reducing the time spent searching for information.
Educate Your Billing Team
- Increases Accuracy in Claim Submissions: Regular training on HCFA form completion, coding updates, and payer-specific guidelines can help billing staff understand the nuances of the submission process, reducing the chances of costly errors.
- Improves Understanding of Coding and Compliance Changes: Coding standards like CPT and ICD-10 are frequently updated, and staying informed is essential. Conducting routine training sessions ensures that the team is aware of these changes and how to apply them effectively.
- Boosts Team Confidence in Billing Processes: A well-trained billing team can work more confidently, reducing hesitation or uncertainty when dealing with complex coding requirements or payer regulations.
- Reduces Error Rates and Speeds Up Claims Processing: With ongoing education, your billing team will make fewer mistakes and submit claims more efficiently, leading to fewer rejections and a faster reimbursement cycle.
Conduct Regular Audits
- Identifies Recurring Issues: Periodic audits help identify recurring errors or bottlenecks in the claims process, such as common coding mistakes, missing information, or procedural missteps that may be leading to denials.
- Enhances Compliance and Reduces Financial Risk: Audits reveal whether your practice is adhering to payer and regulatory requirements, helping you address compliance gaps before they become costly problems.
- Improves Data Quality: By examining claims data and verifying the accuracy of codes, dates, and patient details, audits enhance the quality of your submissions, increasing the chances of successful claim approval.
- Supports Continuous Process Improvement: Auditing highlights areas for improvement in workflows, billing practices, and form completion, leading to fewer rejections and improved cash flow.
Stay Updated on Coding Changes
- Ensures Accurate Coding: Medical billing codes, such as CPT, ICD-10, and HCPCS, are frequently updated to reflect new medical practices, treatments, and diagnoses. Staying current ensures that your claims align with the latest coding standards, reducing the likelihood of denials.
- Prevents Use of Outdated Codes: Using outdated codes is one of the most common reasons for claim rejections. Keeping up with changes means your billing team can avoid these pitfalls and submit claims with correct, up-to-date codes.
- Reduces Reimbursement Delays: Insurance companies may deny or delay claims with incorrect codes. By staying informed of coding updates, your practice can minimize these disruptions and ensure faster reimbursements.
- Simplifies Appeals and Reduces Denials: Knowledge of current codes and billing requirements enables your team to file appeals more accurately, reducing the chance of repeated denials for the same coding issues.
Additional Tips for Avoiding HCFA Errors
- Invest in Quality EMR Software: Many HCFA errors stem from manual data entry mistakes. By implementing reliable EMR software, you can automate the data entry process and minimize common errors.
- Educate Your Billing Team: Ensuring that your team stays informed about coding updates, HCFA form changes, and best practices can significantly reduce errors.
- Conduct Regular Audits: Perform frequent internal audits to catch any inconsistencies or errors before they are submitted.
- Stay Updated on Coding Changes: Medical codes are frequently updated, and healthcare providers should prioritize these updates to ensure compliance and minimize rejections.
Conclusion: Free Resources for HCFA Code Error Resolution
Accessing the right resources is essential for staying current and avoiding errors. Numerous online platforms, including official CMS and other trusted billing education sites, offer free updates and training on HCFA code resolutions. By staying informed and utilizing these resources, you can streamline your billing process, reduce claim rejections, and improve cash flow.
By following these solutions, healthcare providers can ensure smooth claim processing and avoid the pitfalls that come with HCFA form errors. Proper use of these forms not only supports accurate billing but also strengthens compliance and patient care quality. Contact us today so that we can help you submit your errors-free HCFA forms.




