In a Rapidly Changing Healthcare Landscape, Every Claim Counts
In the ever-changing healthcare sector, efficient claims processing is essential. Beyond just cash flow, a smooth claims management process helps you in shaping a great patient experience, boosts organizational stability, and reduces operational strain. This case study explores the journey of PrimeCare LLC and how QZMedx’s targeted strategies improved their billing process, reduced claim denials, and optimized overall efficiency within just two months.
The Challenge: Identifying Roadblocks in PrimeCare LLC’s Claims Management
PrimeCare LLC, a well-established healthcare provider, was encountering key issues that were slowing down their revenue cycle and overburdening administrative resources. Below are the primary challenges:
| Challenges | Impact on Operations |
| High Denial Rates | ~30% of claims denied, leading to delayed revenue and rework for resubmission |
| Complex Coding Issues | Frequent coding errors added rework, slowing claims processing and compliance |
| Lack of Real-Time Analytics | Inability to monitor trends and address issues timely increased processing inefficiency |
| Resource Limitations | High claim volume with limited staff led to burnout and decreased morale |
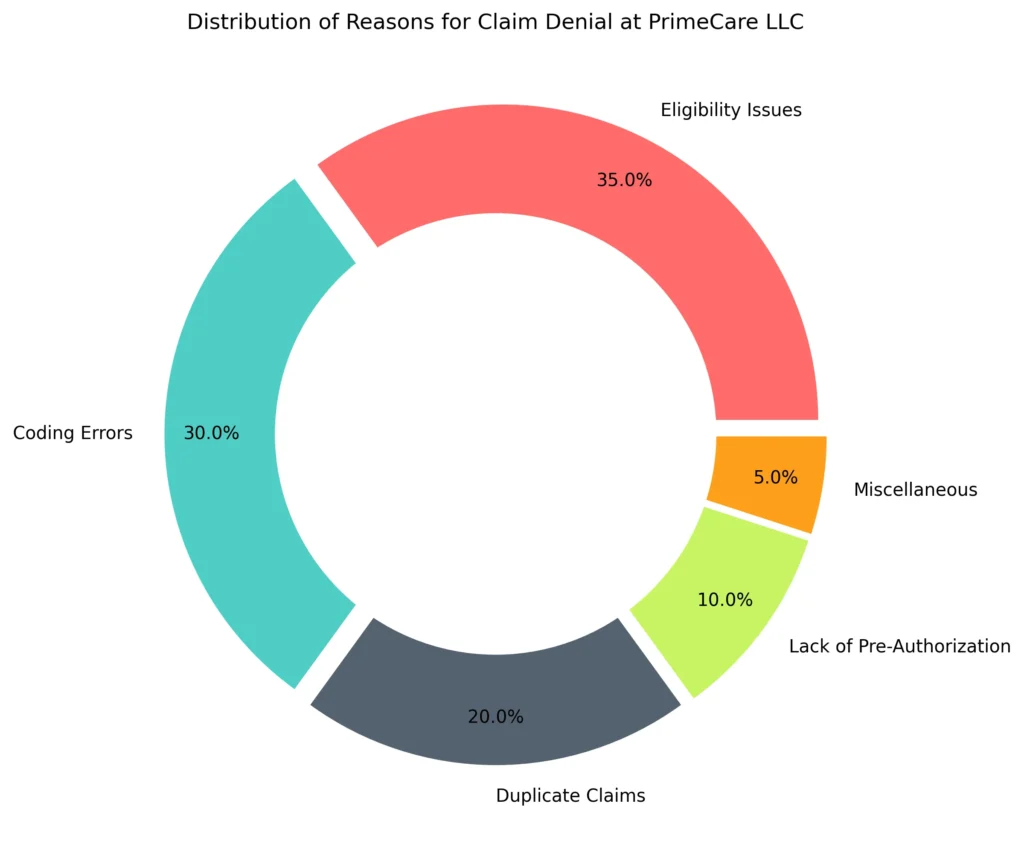
Claim Denial Breakdown
| Reason for Denial | Percentage of Total Denials |
| Eligibility Issues | 35% |
| Coding Errors | 30% |
| Duplicate Claims | 20% |
| Lack of Pre-Authorization | 10% |
| Miscellaneous | 5% |
Our Strategic Approach: A Tailored, Multi-Stage Solution
To address PrimeCare’s challenges, QZMedx developed a comprehensive approach that included in-depth analysis, advanced technology, and hands-on training.
1. Detailed Claims Analysis: Getting to the Root of the Problem
Our initial step was a deep-dive analysis into PrimeCare’s claims data and processes. This phase included:
- Historical Data Review: Analyzed years of claims data to identify root causes of denials.
- Engagement with Billing Staff: Conducted workshops with the billing team to understand workflow challenges and needs.
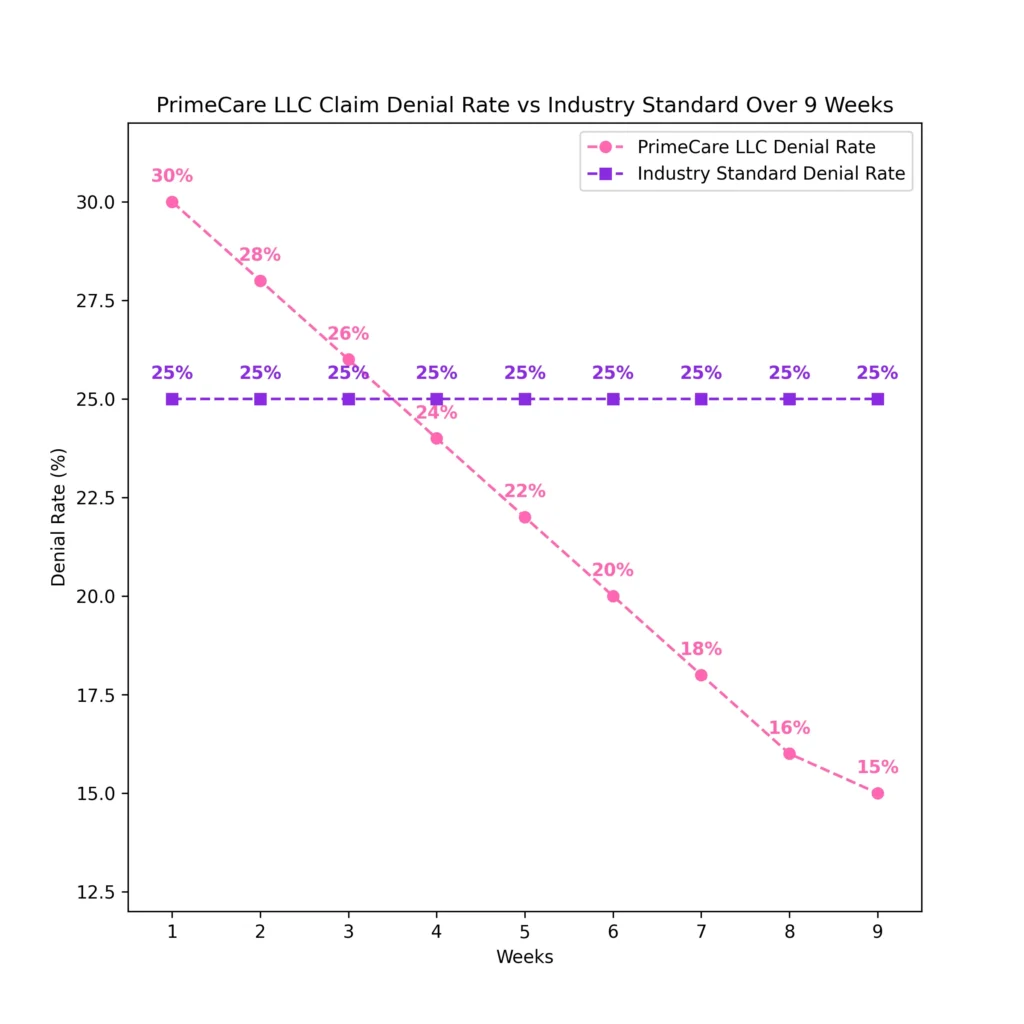
- Benchmarking Against Industry Standards: Compared PrimeCare’s denial and processing metrics to healthcare standards, highlighting key improvement areas.
| Metric | PrimeCare’s Rate (Before) | Industry Standard |
| Claim Denial Rate | 30% | 10-15% |
| Average Processing Time | 14 days | 10 days |
| Coding Error Rate | 20% | <10% |
2. Technology Implementation: Bringing Innovation to Claims Processing
Using cutting-edge technology, we transformed PrimeCare’s approach to claims management:
- Automated Coding Solutions: Implemented AI-based coding software to reduce errors and speed up claims submissions.
- Real-Time Analytics Dashboard: Custom dashboard providing immediate insights into claims status, denial reasons, and performance metrics.
- Integrated Workflow Management: Enhanced communication among team members through a centralized workflow system.
| Technology Component | Impact |
| Automated Coding Solutions | 30% reduction in coding errors |
| Real-Time Analytics Dashboard | 25% improvement in claims processing speed |
| Integrated Workflow Management | 20 hours saved per week on administrative tasks |
3. Training and Support: Empowering PrimeCare’s Billing Team
Recognizing the importance of human expertise, we provided extensive training to help staff adapt to new technologies and methods.
- Workshops on Best Practices: Educated staff on coding, claims submission, and denial management best practices.
- Ongoing Technical Support: Dedicated support team available for troubleshooting and guidance.
- Continuous Feedback Mechanism: Established channels for staff to communicate challenges and suggest improvements.
The Results: Tangible Improvements for PrimeCare LLC
With QZMedx’s solutions in place, PrimeCare LLC saw significant, measurable improvements within just 60 days. Here’s a breakdown of the key achievements:
Outcome Highlights
| Key Metric | Improvement |
| Denial Rate Reduction | 40% |
| Coding Accuracy Improvement | 30% |
| Claims Processing Speed Increase | 25% |
| Revenue Cycle Performance Boost | 15% |
Financial and Operational Impact
| Metric | Before QZMedx | After QZMedx | Change |
| Claim Denial Rate | 30% | 18% | -40% |
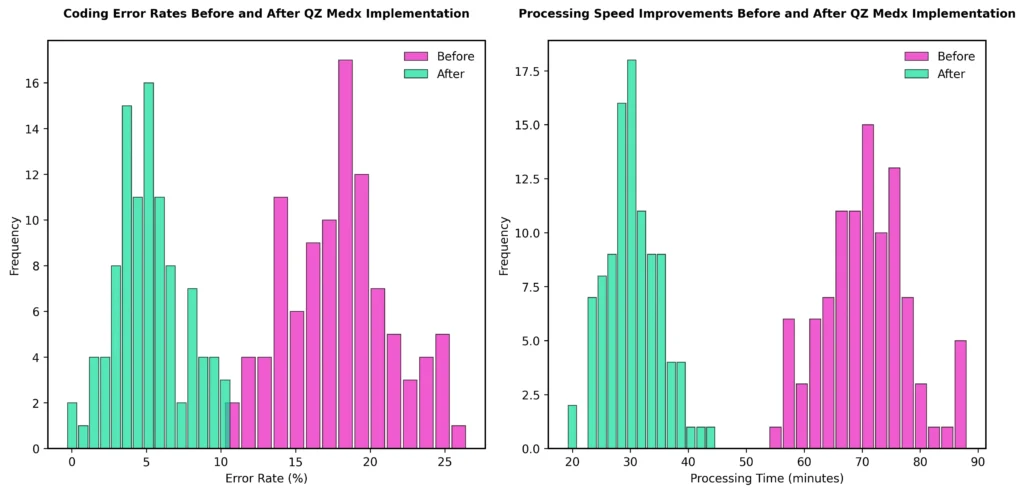
| Average Coding Error Rate | 20% | 14% | -30% |
| Average Processing Time (Days) | 14 days | 10.5 days | -25% |
| Cash Flow Improvement | Baseline | +15% | +15% |
Key Improvements
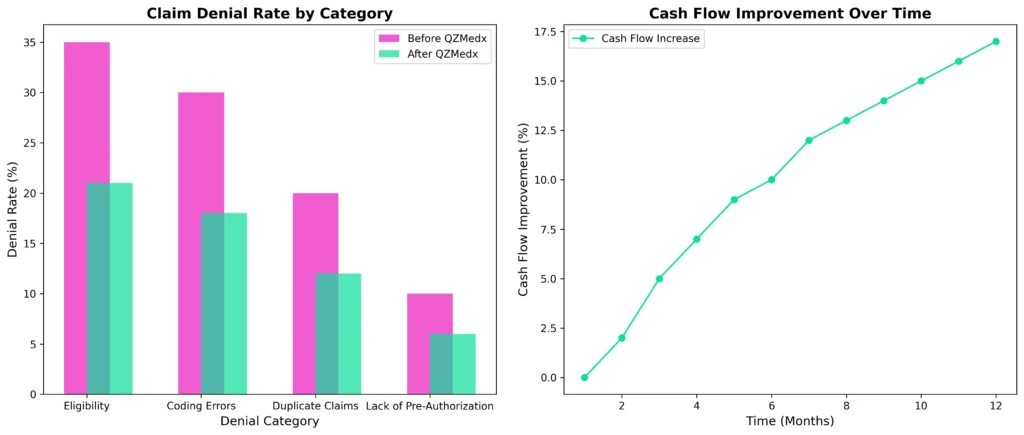
1. Significant Drop in Claim Denials
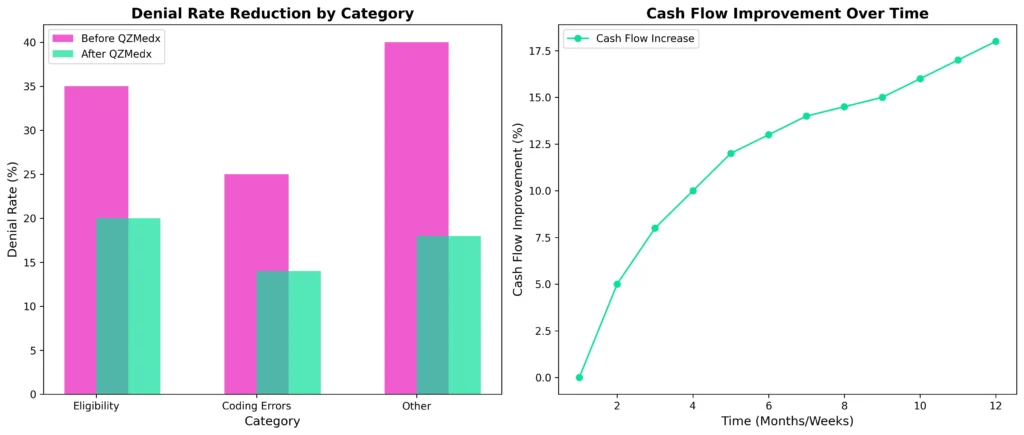
By implementing proactive denial management, PrimeCare saw a 40% reduction in claim denials, which enabled a more predictable cash flow and freed up administrative resources.
2. Enhanced Coding Accuracy
With automated coding, PrimeCare’s error rate dropped by 30%, which significantly streamlined claims processing and improved compliance.
3. Faster Claims Processing
The real-time analytics dashboard helped reduce claim processing time by 25%, meaning claims were processed and paid faster.
4. Boosted Financial Performance
A 15% increase in revenue cycle performance allowed PrimeCare to stabilize its financial health and reinvest in quality patient care.
Visualizing Key Performance Improvements
1. Claim Denial Rate by Category
| Denial Category | Before QZMedx | After QZMedx |
| Eligibility | 35% | 21% |
| Coding Errors | 30% | 18% |
| Duplicate Claims | 20% | 12% |
| Lack of Pre-Authorization | 10% | 6% |
2. Cash Flow Increase (Line Chart)
Below chart tracks cash flow growth month-over-month after implementing QZMedx’s solutions.
Concluding Insights: A Case Study in Claims Optimization Success
The collaboration between QZMedx and PrimeCare LLC is a powerful example of how a targeted approach to claims management can deliver transformative results. By addressing PrimeCare’s unique challenges with advanced technology, focused training, and continuous support, we helped them achieve:
- 40% reduction in claim denials
- 25% faster processing speed
- 30% improvement in coding accuracy
These improvements have strengthened PrimeCare’s financial foundation, streamlined their operations, and enhanced patient satisfaction.
QZMedx: Your Partner in Claims Management Excellence
At QZMedx, we specialize in empowering healthcare providers like PrimeCare LLC to overcome billing challenges and improve financial performance. With a commitment to continuous innovation and personalized solutions, we’re here to help transform the medical billing landscape for healthcare providers across the country.