Who is Ayman Care?
Ayman Care, a leader in personalized healthcare services, provides primary care, specialty consultations, and preventive health programs. Located in an urban hub, their mission is clear: to improve patients’ quality of life through compassionate, high-quality care. But, like many healthcare providers, Ayman Care faced challenges in managing billing processes efficiently, impacting both patient satisfaction and revenue.
Pain Points That Impacted Ayman Care’s Success
For Ayman Care, managing effective medical billing wasn’t just an administrative necessity—it was integral to their reputation, financial stability, and ability to serve patients effectively. However, certain persistent challenges made it difficult to meet these goals.
1. High Claim Denial Rates: Slowing Revenue and Increasing Administrative Burden
One of Ayman Care’s most pressing issues was a high rate of claim denials from insurance providers. Common reasons for denials included coding inaccuracies, incomplete documentation, and occasionally, discrepancies in patient eligibility data. These denials had a twofold impact:
- Revenue Delays: Denials significantly slowed down cash flow, leaving funds tied up in appeals and corrections. This hindered Ayman Care’s ability to invest back into the practice, affecting everything from staffing to facility improvements.
- Administrative Strain: With a large volume of claims requiring follow-up, the administrative team was stretched thin. Time and resources that could have been used to improve patient care were instead diverted to managing denials and resubmitting claims.
Reducing claim denial rates was essential to ensure that revenue was collected promptly and that staff could focus on higher-value tasks.
2. Inefficient, Manual Billing Processes: Increasing Errors and Time Wasted
Ayman Care’s billing operations were heavily reliant on manual processes. From data entry to coding and claim submission, tasks were often handled by hand, increasing the potential for human error and slowing down workflows. These inefficiencies led to:
- Frequent Errors: Manual entry left room for mistakes in patient information and billing codes, both of which were common reasons for claim denials.
- Excessive Time Consumption: Staff had to spend substantial time on repetitive, low-value tasks like data entry. This diverted their attention away from more strategic or patient-focused duties, which ultimately impacted service quality.
By introducing automation to these processes, Ayman Care could reduce errors and improve overall operational efficiency, freeing up staff to focus on patient care.
3. Lack of Billing Transparency: Undermining Patient Trust and Satisfaction
Patients frequently expressed confusion over billing statements, which were often unclear and difficult to understand. This lack of transparency led to:
- Patient Frustration and Anxiety: Patients want clear explanations for the charges on their statements. Without transparent billing, patients can feel frustrated or distrustful, especially when they don’t understand what they’re being charged for.
- Increased Inquiries and Complaints: Unclear statements led to a high volume of billing-related inquiries, creating additional administrative burden for the billing team. Staff had to spend time clarifying charges rather than focusing on more proactive tasks.
Improving transparency in billing was critical to building patient trust and reducing the administrative workload, creating a smoother experience for both patients and staff.
4. Limited Revenue Cycle Insights: Preventing Proactive Decision-Making
Ayman Care lacked comprehensive insights into their revenue cycle, making it difficult to track financial performance, identify trends, or pinpoint areas that needed improvement. This lack of oversight led to:
- Missed Opportunities for Improvement: Without the ability to track key metrics, Ayman Care’s management was unable to take corrective action proactively. For instance, they couldn’t easily identify specific claim types or payers contributing to the highest denial rates.
- Reactive Problem Solving: Rather than spotting issues early, Ayman Care’s team often had to react to problems after they became critical. This limited their ability to set meaningful goals, optimize revenue collection, and streamline operations effectively.
Implementing analytics and reporting tools could empower the team with actionable insights, allowing them to make data-driven decisions and continuously improve their revenue cycle management.
5. Administrative Staff Overload: Impacting Staff Morale and Patient Care Quality
Finally, the sheer volume of administrative tasks associated with billing had a tangible effect on staff morale and performance. The billing team was stretched thin, which led to:
- Decreased Efficiency and Increased Errors: As the workload increased, staff struggled to keep up, leading to burnout and a higher likelihood of mistakes in claims processing.
- Reduced Focus on Patient Care: Overwhelmed by administrative duties, the team had limited time to engage in patient interactions or handle other essential functions. This created a vicious cycle where inefficiencies in billing began to impact the overall quality of care and patient satisfaction.
By alleviating the administrative burden, Ayman Care could allow its team to redirect energy and focus back toward patient care, reducing burnout and fostering a more positive work environment.
Innovative Solutions by QZ Medx
| Solution | Description | Key Metrics Impacted |
| Comprehensive Claims Management | Targeted denial reduction strategies, optimized coding and follow-ups for denied claims | Claim denial rate, revenue collection time |
| Streamlined Billing Processes | Automation of data entry and billing code management through state-of-the-art software | Billing task time reduction, error rate |
| Necessary Patient Communication | Redesigned billing statements with a patient portal for better access and transparency | Patient satisfaction, inquiry reduction |
| Revenue Cycle Analytics | Real-time KPI dashboards for better revenue cycle tracking and decision-making | Days in AR, approval rates, trends |
| Staff Training and Support | Comprehensive training sessions and ongoing support for effective use of new tools | Staff confidence, productivity increase |
Before-and-After Impact Analysis
To provide a clearer picture of the improvements made, here are metrics before and after the intervention by QZ Medx.
| Metric | Before Intervention | After Intervention | Percentage Improvement |
| Claim Denial Rate | 18% | 12.6% | 30% reduction |
| Billing Task Time | 45 hours/week | 27 hours/week | 40% reduction |
| Patient Billing Inquiries | 90 inquiries/month | 50 inquiries/month | 44% reduction |
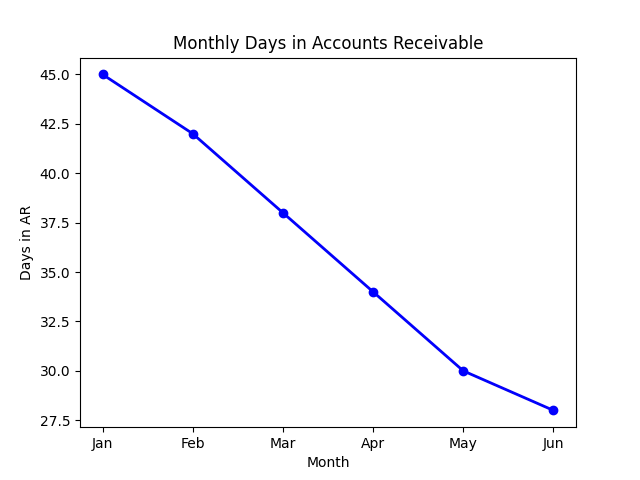
| Days in Accounts Receivable (AR) | 45 days | 30 days | 33% improvement |
| Staff Satisfaction Score | 70/100 | 88/100 | 26% increase |
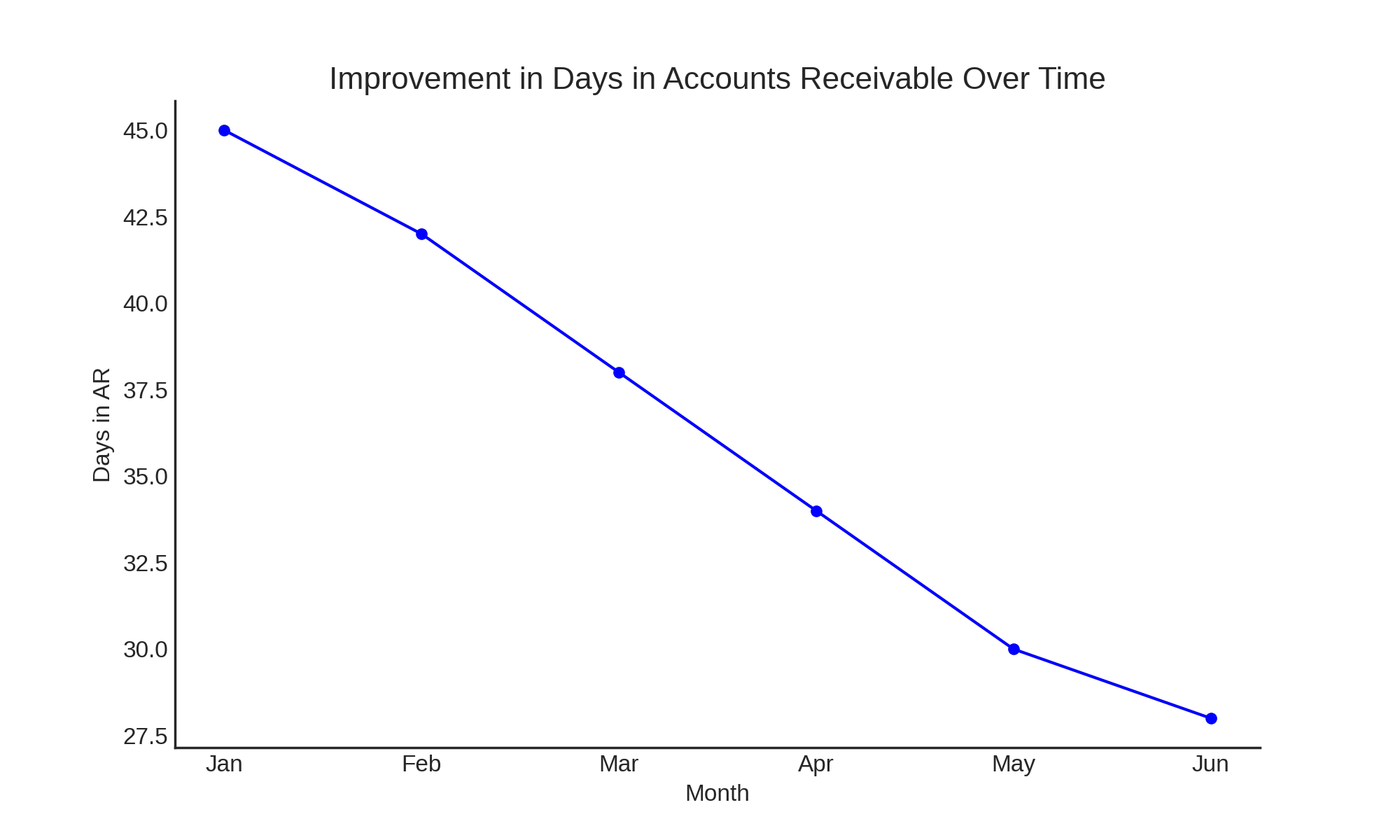
Transformative Results and Key Performance Improvements
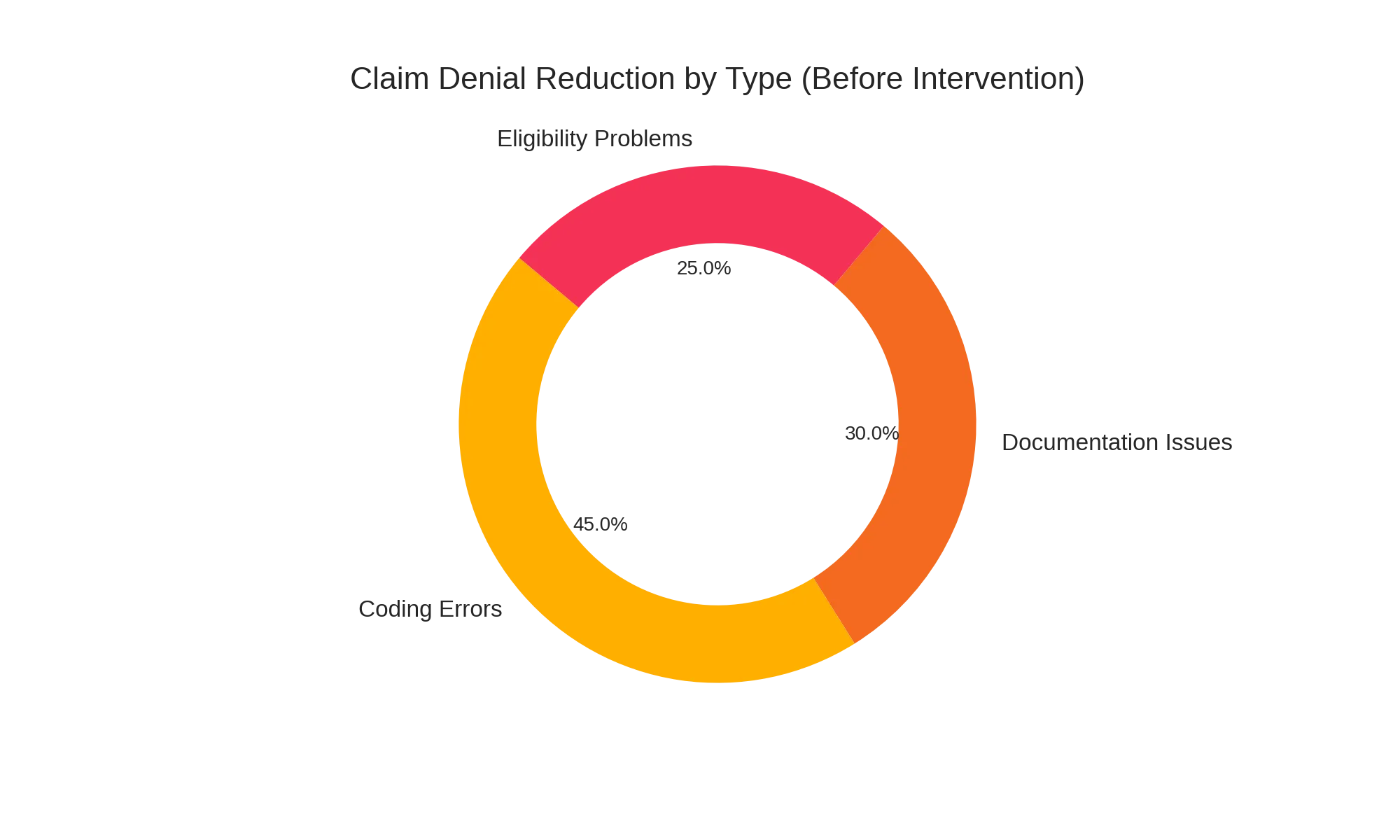
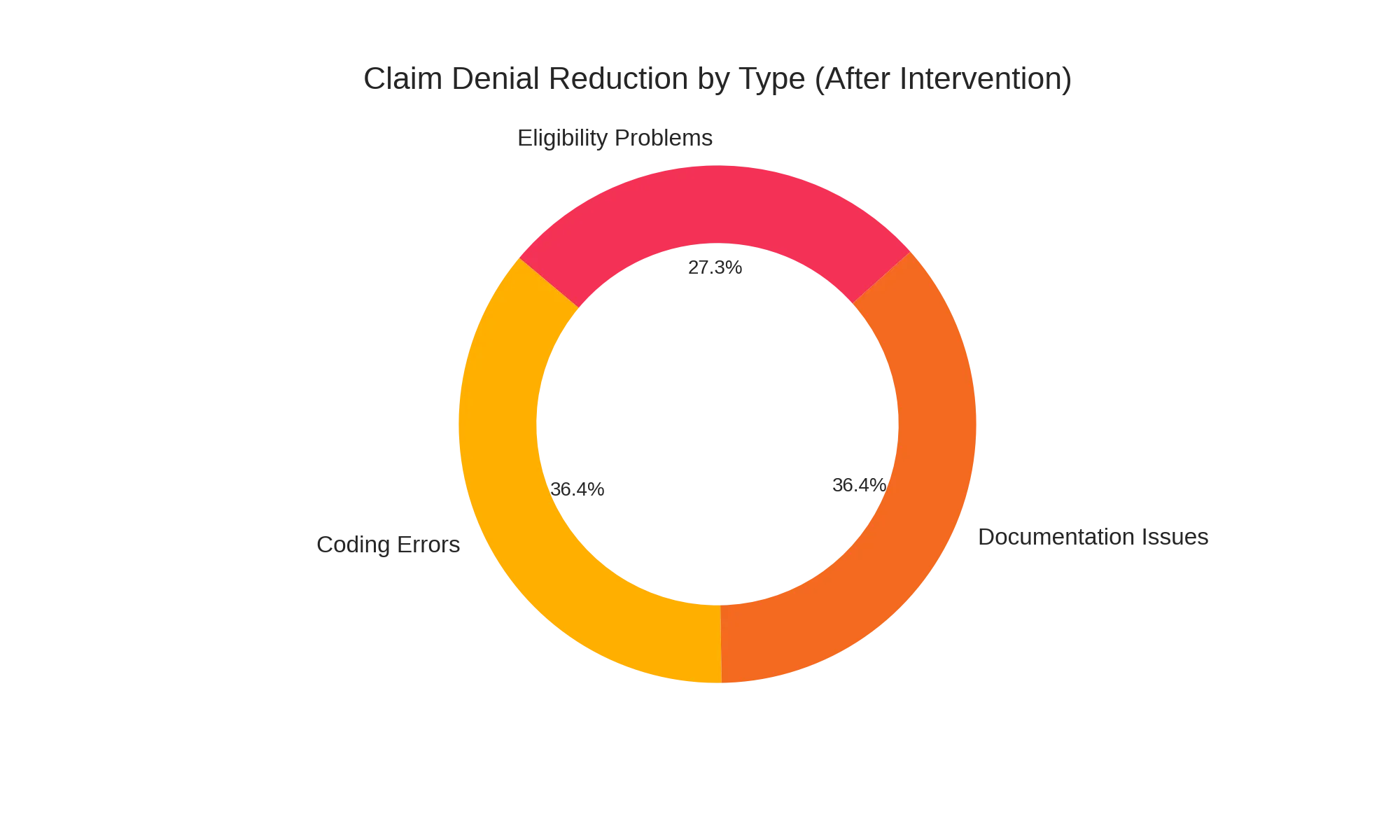
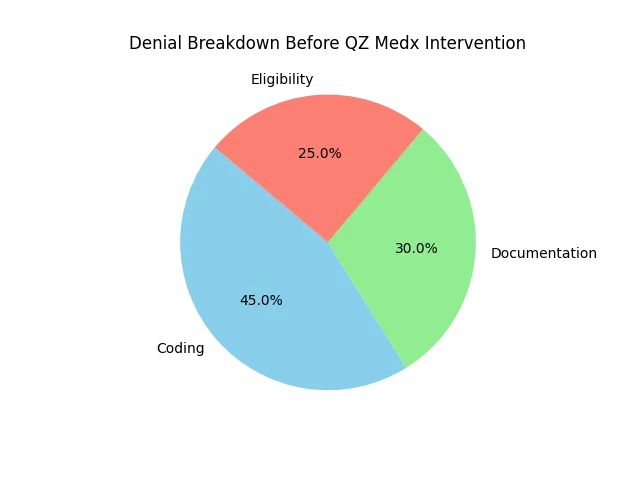
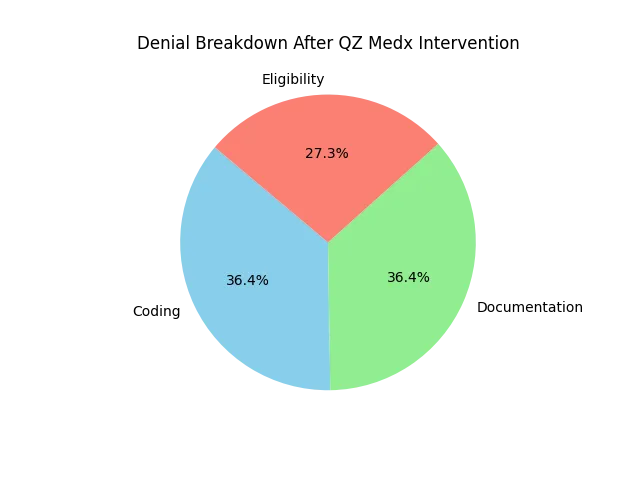
Claim Denial Rates: A 30% Reduction in Denials
Through optimized coding practices, Ayman Care’s denial rate dropped significantly. As depicted in the chart below, coding errors accounted for 45% of denials prior to QZ Medx’s intervention, but improved documentation and focused follow-ups reduced this rate.
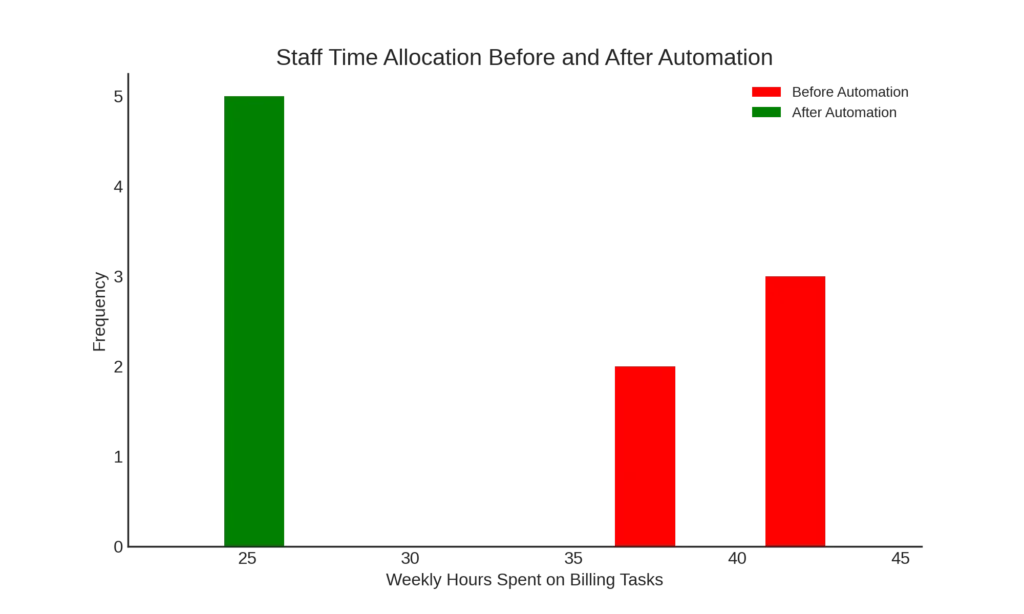
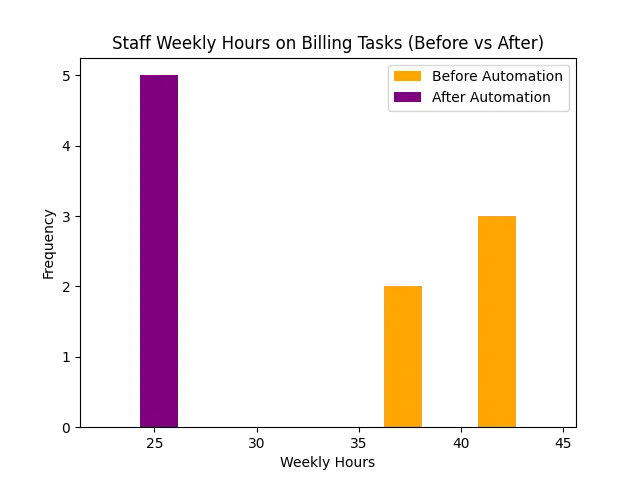
Billing Efficiency Gains: 40% Reduction in Time Spent on Billing Tasks
With streamlined billing software, Ayman Care’s administrative time was cut nearly in half. This allowed more time for patient engagement, directly enhancing patient satisfaction scores.
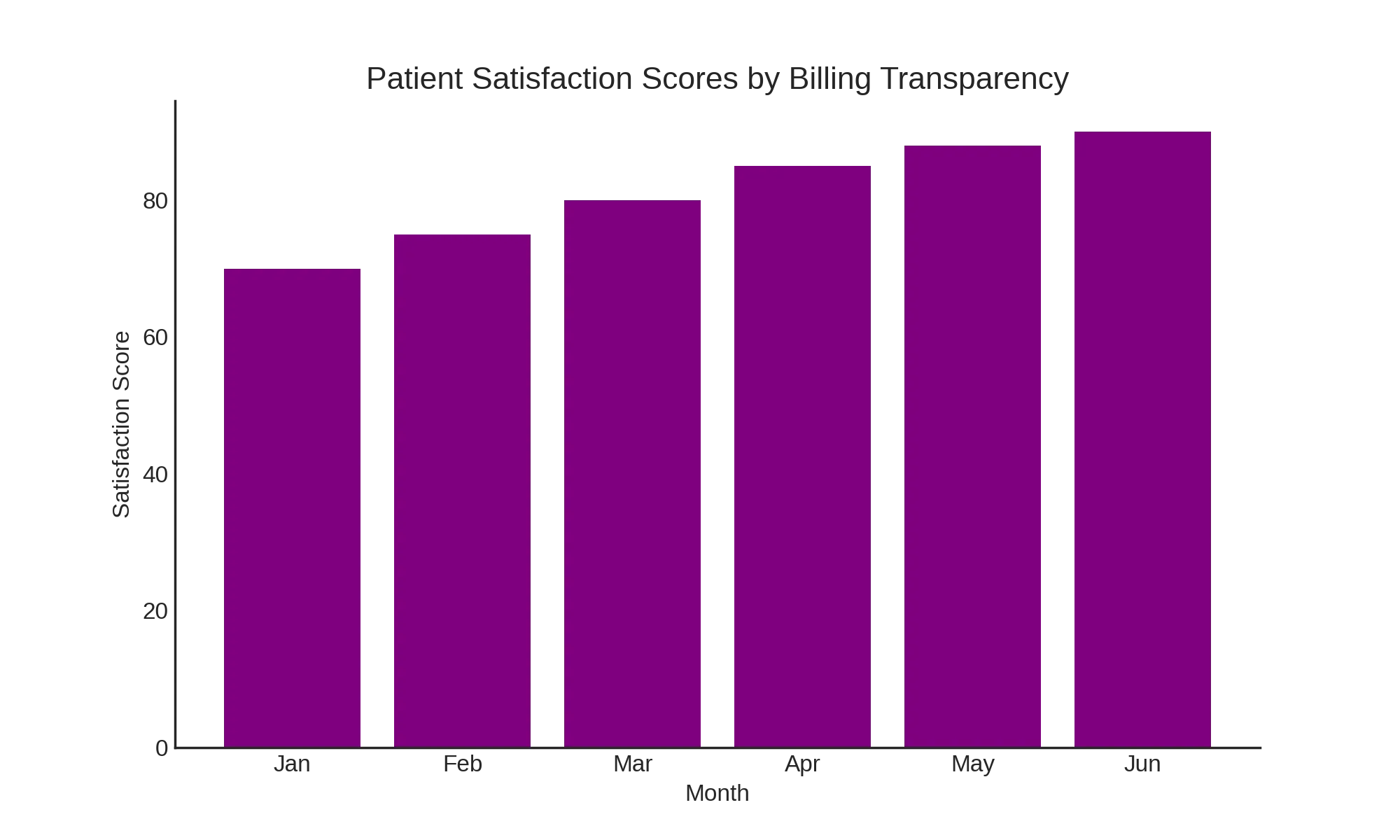
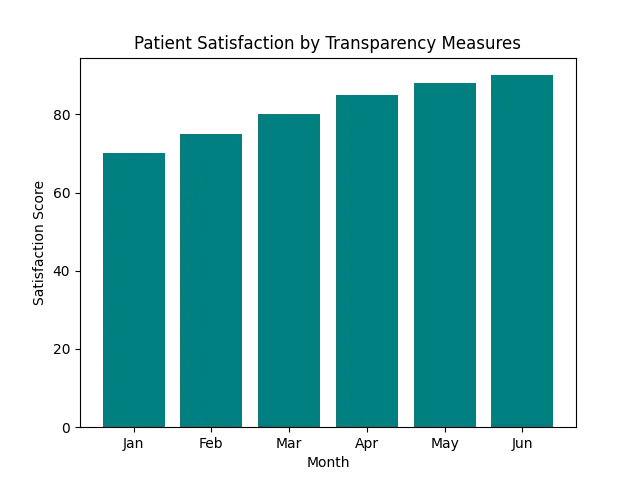
Increased Transparency and Patient Satisfaction: 44% Reduction in Billing Inquiries
Newly designed billing statements and a user-friendly portal improved transparency. Patients now had easier access to their statements, resulting in a significant drop in billing-related inquiries and a boost in overall satisfaction.
Conclusion: A Successful Transformation for Ayman Care
Empowering Ayman Care
The partnership between Ayman Care and QZ Medx showcases how dedicated interventions in medical billing can transform operations, reduce costs, and boost patient satisfaction. The results speak for themselves: reduced denial rates, quicker revenue cycles, and empowered staff—all enabling Ayman Care to focus on delivering outstanding patient care.
Looking Forward: Ongoing Excellence in Billing Operations
As Ayman Care grows, the streamlined processes and data insights provided by QZ Medx will continue to support them in their mission, ensuring sustainable improvements and setting a high standard in healthcare billing excellence.