When checking in the U.S. healthcare system, understanding whether you need inpatient or outpatient care can make a world of difference. These terms aren’t just medical jargon—they directly impact where you receive care, the cost of that care, and how your insurance will cover it.
This blog post will break down the differences between inpatient or outpatient hospital care, helping you make informed decisions about your healthcare needs.
What Is Inpatient and Outpatient Care?
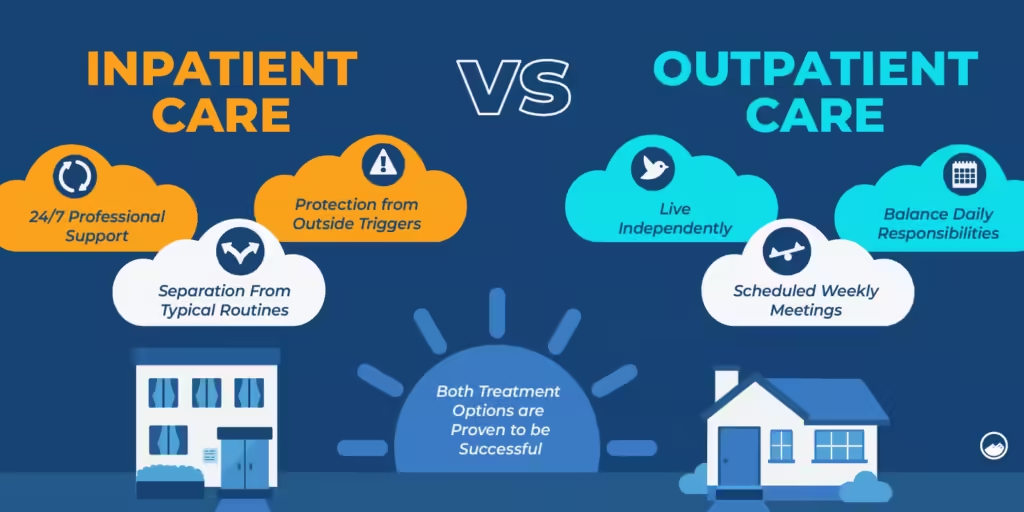
Inpatient Care
Inpatient care requires admission to a hospital or healthcare facility for at least one overnight stay. Patients undergoing inpatient care are under continuous monitoring by healthcare professionals. This type of care often involves severe medical conditions or major surgeries that require close supervision and specialized treatment.
Examples of inpatient care include:
- Childbirth: A mother delivering a baby may stay in the hospital for 2–4 days depending on the delivery method.
- Heart attacks or strokes: Patients often require prolonged stays for monitoring and rehabilitation.
- Major surgeries: Procedures like joint replacements or organ transplants involve extensive recovery periods, often necessitating days in the hospital.
Outpatient Care
Outpatient care refers to medical services that do not require an overnight hospital stay. Patients visit a healthcare provider, undergo the necessary procedure or treatment, and return home the same day.
Examples of outpatient care include:
- Routine screenings: Mammograms and colonoscopies are often conducted on an outpatient basis.
- Minor surgeries: Procedures like mole removal, cataract surgery, or tonsillectomies.
- Preventive care: Annual physicals or flu shots.
Key Differences Between Inpatient and Outpatient Care
1. Duration of Stay
The most significant distinction lies in the duration of the stay. Inpatient care involves at least one overnight stay, whereas outpatient care allows patients to leave the same day.
2. Costs and Insurance Coverage
According to HealthCare.gov, the average cost of a three-day inpatient hospital stay is around $30,000, whereas an outpatient visit averages $500. This disparity is due to the additional expenses associated with inpatient care, including room charges, meals, and 24/7 monitoring.
Insurance coverage for both care types varies based on your plan:
- For inpatient care, Medicare Part A covers hospital services, but you may face high deductibles.
- For outpatient care, Medicare Part B often covers routine tests and screenings, but copayments apply.
Tip: Patients can lower costs by choosing outpatient facilities for minor procedures when medically appropriate. A Blue Cross Blue Shield study revealed that routine care is 58% cheaper at a doctor’s office than in a hospital.
3. Type of Services Provided
- Inpatient: Intensive care, rehabilitation, or life-threatening conditions that need constant medical attention.
- Outpatient: Diagnostic tests, preventive screenings, and minor procedures requiring minimal recovery time.
How to Decide: Inpatient vs. Outpatient
The decision to opt for inpatient or outpatient care isn’t always up to the patient—it largely depends on the nature of the medical issue and your physician’s recommendation.
Factors That Influence the Choice:
- Severity of the Condition:
- A heart attack will almost always require inpatient care.
- A sprained ankle may be treated on an outpatient basis.
- Complexity of the Procedure:
- Surgeries like hip replacements need hospital stays.
- Mole removal or dental procedures are often done outpatient.
- Insurance and Cost Considerations:
- If you’re on a high-deductible health plan, outpatient care may help lower expenses.
Real-Life Example:
Consider Jessica, a 45-year-old from Chicago. She recently underwent a colonoscopy at an outpatient center. Since it was preventive, her insurance covered 100% of the cost. A week later, her husband suffered a heart attack and was admitted as an inpatient. His three-day hospital stay cost over $20,000. The family’s out-of-pocket maximum was reached, which limited their financial burden, but it underscored how drastically costs can differ.
Examples of Procedures in Each Setting
Inpatient Procedures
- Childbirth (2–4 days stay).
- Heart bypass surgery (average 5–7 days stay).
- Rehabilitation for substance use disorders.
Outpatient Procedures
- Dental surgeries (e.g., wisdom tooth extraction).
- Imaging services (e.g., X-rays, MRIs).
- Cancer treatments like chemotherapy.
The Cost Factor: Why It Matters
Understanding the financial impact of inpatient and outpatient care is crucial, especially in the U.S., where healthcare costs are notoriously high.
- Inpatient Costs: Include not just the procedure but also administrative fees, room charges, meals, and 24/7 medical staff.
- Outpatient Costs: Limited to the procedure, physician fees, and any necessary medications or follow-ups.
Tips for Reducing Healthcare Costs:
- Compare Facilities: An MRI can cost $1,200 at a hospital but as low as $400 at an outpatient imaging center.
- Know Your Insurance Plan: Take advantage of preventive care benefits often covered fully by insurance.
- Ask About Alternatives: If your condition allows, ask your doctor whether outpatient treatment is a viable option.
Why It’s Important to Know the Difference
For patients like you, understanding the distinction between inpatient and outpatient care offers more control over medical decisions and costs. It allows for better planning when choosing a health plan, anticipating out-of-pocket expenses, and navigating insurance claims.
For example, a family planning for childbirth can compare costs and facilities to make an informed decision between a hospital’s labor ward or a birthing center offering outpatient services.
Inpatient vs. Outpatient Costs
Why Are Costs Different?
The cost disparity between inpatient and outpatient care lies in the nature of the services provided. Inpatient care is resource-intensive, involving 24/7 monitoring, room charges, and meals, while outpatient care limits costs to the procedure or visit itself.
- Inpatient Costs Include:
- Room and board fees (hospital beds cost an average of $2,000 per day).
- Administrative fees for admission and discharge.
- Nursing and medical staff costs.
- Diagnostic and laboratory tests conducted during the stay.
- Outpatient Costs Include:
- Procedure or diagnostic test fees.
- Doctor’s or specialist’s consultation charges.
- Medications or follow-up care costs.
Real-Life Example:
A three-day inpatient hospital stay costs about $30,000 on average in the U.S., while an outpatient colonoscopy might cost $2,000 at most, depending on the facility.
Inpatient vs. Outpatient Insurance
How Insurance Covers Each
Insurance plans handle inpatient and outpatient care differently, often splitting coverage between Medicare Part A and Part B or similar provisions in private insurance.
- Inpatient Care:
- Covered under Medicare Part A or equivalent private insurance plans.
- Includes hospitalization costs like room charges, treatments, and nursing care.
- Often subject to higher deductibles due to the higher cost of care.
- Outpatient Care:
- Covered under Medicare Part B or private insurance outpatient provisions.
- Typically includes diagnostic tests, minor surgeries, and preventive screenings.
- Copayments and coinsurance often apply but at significantly lower rates than inpatient care.
Tips for Maximizing Coverage:
- Always confirm whether a procedure requires admission as an inpatient; misclassification can result in unexpected costs.
- Choose in-network outpatient facilities for lower copayments.
- Review your deductible status annually to determine if outpatient care is more cost-effective near year-end.
What Is Inpatient Care?
Inpatient care refers to treatments or medical interventions requiring admission to a hospital or similar facility for at least one overnight stay.
Characteristics of Inpatient Care:
- 24/7 monitoring by healthcare professionals.
- Treatment for severe conditions, such as strokes or traumatic injuries.
- Comprehensive services, including meals, medications, and rehabilitation plans.
- Often follows emergency admissions or planned surgeries.
Outpatient Services Examples
Outpatient services are procedures or treatments that do not require an overnight stay. They are ideal for minor or routine medical issues that allow patients to recover at home.
Common Outpatient Services:
- Diagnostic Screenings: Mammograms, colonoscopies, and X-rays.
- Minor Surgical Procedures: Cataract removal, mole excision, and hernia repairs.
- Physical Therapy and Rehabilitation: Short-term or ongoing therapy for recovery.
- Routine Check-Ups: Annual physicals and specialist consultations.
- Preventive Treatments: Vaccinations and wellness screenings.
Inpatient Hospital Meaning
An inpatient hospital stay involves being formally admitted to a healthcare facility for treatment that necessitates at least one overnight stay.
Key Features of Inpatient Hospitals:
- Dedicated wards or units for specialized care (e.g., ICU, maternity, or oncology).
- Access to advanced diagnostic tools, surgical facilities, and emergency interventions.
- Continuous care provided by interdisciplinary teams of doctors, nurses, and specialists.
Outpatient Hospital Meaning
Outpatient hospital services allow patients to visit a medical facility for diagnosis or treatment without requiring an overnight stay.
Examples of Outpatient Hospital Care:
- Day surgeries conducted in specialized outpatient surgical centers.
- Emergency room visits for minor injuries that do not result in admission.
- Outpatient imaging services, such as MRIs or CT scans.
Difference Between Inpatient and Outpatient Prescriptions
The setting of care impacts how prescriptions are issued and managed.
Inpatient Prescriptions:
- Administered directly by medical staff during the hospital stay.
- Part of a broader treatment plan monitored in real-time.
- Costs often bundled with hospital charges.
Outpatient Prescriptions:
- Prescribed for home use following diagnosis or minor procedures.
- Includes refills managed by pharmacies or specialist follow-ups.
- Typically requires separate payment, even with insurance, through copayments.
Inpatient Services Examples
Inpatient services cater to severe medical conditions requiring comprehensive care.
Examples of Inpatient Services:
- Major Surgeries: Organ transplants, cardiac bypass, or joint replacements.
- Acute Care: Treating conditions like heart attacks or pneumonia.
- Childbirth: Including Cesarean sections or complicated deliveries.
- Rehabilitation: Post-surgery physical therapy or treatment for substance use disorders.
- Mental Health Interventions: Long-term care for severe psychological conditions.
Conclusion
Inpatient and outpatient care each serve critical roles in the healthcare system, tailored to the severity and complexity of medical conditions. Understanding these differences not only helps patients manage costs but also ensures they receive the appropriate care in the right setting.
So, the next time you or a loved one face a medical decision, remember:
- Inpatient care is for serious, monitored conditions requiring a hospital stay.
- Outpatient care offers a convenient, cost-effective solution for minor or routine issues.
Stay informed, ask questions, and advocate for your health. By doing so, you can make the best choices for your medical and financial well-being. Stay tuned with QZMedx for more info!