As we step into 2025, the healthcare landscape continues to evolve at an unprecedented pace. This evolution is particularly evident in the fields of medical billing and coding, where technology, regulatory changes, and shifting care models are reshaping how healthcare providers operate. For medical practices of all sizes, understanding these trends is not just beneficial; it’s essential for maintaining compliance, optimizing revenue cycles, and ensuring timely reimbursement for services rendered.
In this article, we will explore the top medical billing and coding trends anticipated for 2025. By staying informed about these developments, healthcare providers can better position themselves to thrive in an increasingly complex environment.
1. Increased Focus on AI and Automation
Artificial intelligence (AI) and automation are revolutionizing medical billing and coding processes. These technologies are no longer just concepts of the future; they are actively being integrated into everyday operations to enhance efficiency and accuracy.
What to Expect:
- Claim Scrubbing: AI algorithms can automatically identify errors and inconsistencies in claims before submission, significantly reducing the likelihood of denials.
- Code Assignment: AI tools assist coders in selecting the most accurate codes based on comprehensive medical documentation.
- Prior Authorization: Automating the prior authorization process can save time and resources, allowing staff to focus on more complex tasks.
Impact: The integration of AI and automation is expected to lead to a reduced administrative burden, faster claim processing times, and improved overall revenue cycle efficiency.
How QZ Medx Can Help: At QZ Medx, we utilize cutting-edge technology to streamline your clinic’s operations while reducing overhead costs by up to 45%. Our solutions are designed to enhance your practice’s efficiency without compromising quality.
2. Rise of Value-Based Care and Its Impact on Coding
The healthcare industry is increasingly shifting from traditional fee-for-service models to value-based care (VBC) approaches that prioritize patient outcomes and quality of care. This transition has profound implications for medical coding practices.
What to Expect:
- More Detailed Coding: Accurate coding is essential for tracking patient outcomes and demonstrating the value of care provided.
- Emphasis on Quality Reporting: Coders will play a crucial role in capturing data necessary for quality reporting programs.
- Focus on Risk Adjustment: Properly coding patient diagnoses will be critical for risk adjustment within VBC models.
Impact: This shift will necessitate greater coding expertise, increased emphasis on thorough documentation, and a closer relationship between coding accuracy and reimbursement rates.
How QZ Medx Can Help: Our team of certified coders offers personalized ICD-10, CPT, and HCPCS coding services. We stay updated with the latest coding guidelines to ensure precise code assignment and minimize claim rejections.
3. Enhanced Cybersecurity Measures
As healthcare becomes increasingly digitized, protecting sensitive patient data from cyber threats is paramount. The industry remains a prime target for cyberattacks due to the valuable nature of health information.
What to Expect:
- Stricter Data Security Regulations: Anticipate heightened scrutiny regarding compliance with HIPAA regulations.
- Investment in Cybersecurity Infrastructure: Medical practices will need to invest in robust security measures to safeguard against data breaches.
- Employee Training on Cybersecurity Best Practices: Educating staff about potential threats like phishing scams is essential for maintaining security.
Impact: While compliance with cybersecurity measures may increase operational costs, it significantly reduces the risk of data breaches and associated financial losses.
How QZ Medx Can Help: Entrust your billing needs to us; our Revenue Cycle Management (RCM) processes are fully HIPAA compliant. Our team remains vigilant about regulatory changes to ensure your billing operations are secure.
4. Changes in CPT and ICD-10 Coding Guidelines
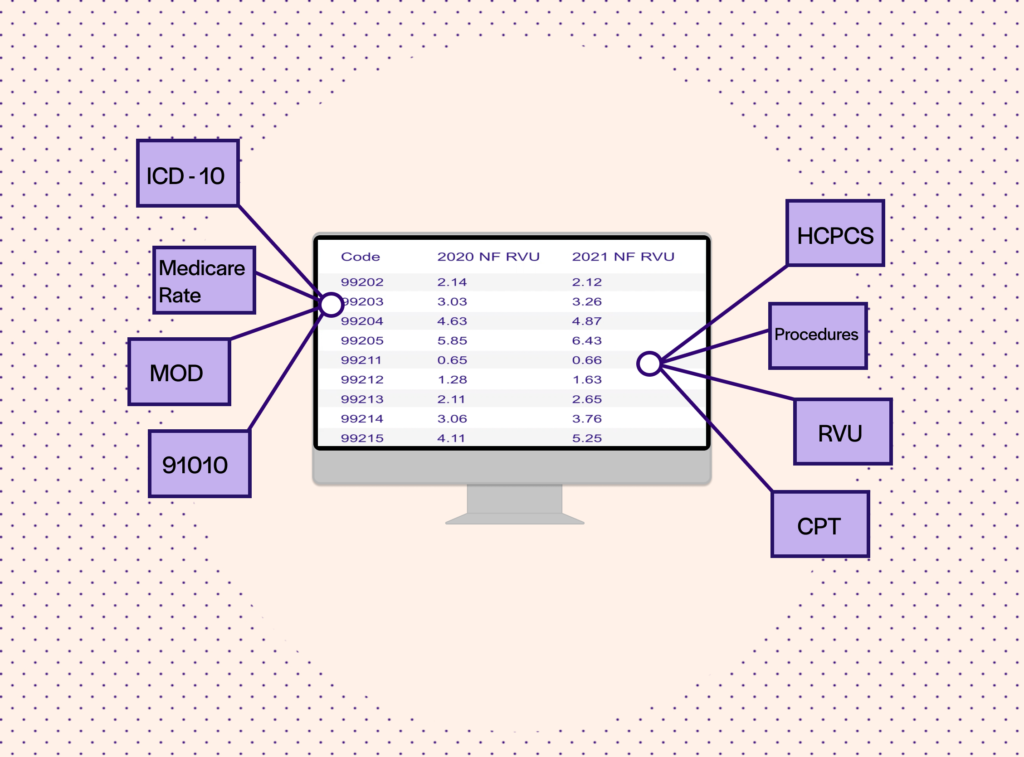
Annual updates to CPT (Current Procedural Terminology) and ICD-10 (International Classification of Diseases) coding guidelines are a staple in medical billing and coding. Staying informed about these changes is crucial for accurate medical billing and coding practices.
What to Expect:
- New Codes: Be prepared for new codes that reflect advancements in medical technology and procedures.
- Revised Codes: Existing codes may undergo revisions or deletions, necessitating ongoing education for coders.
- Clarifications and Updates: Regular updates will require coders to stay informed about changes in guidelines.
Impact: There will be an ongoing need for coder education and training. Failure to implement updates correctly could lead to increased coding errors.
How QZ Medx Can Help: We provide insights into significant changes in CPT codes for 2025 and their implications for medical billing practices. Our experts ensure that your team is well-prepared for these updates.
5. Telehealth Billing and Coding Nuances
The rise of telehealth has transformed healthcare delivery but also introduced complexities in billing and coding that require specialized knowledge.
What to Expect:
- Evolving Telehealth Coding Guidelines: Payers are continually updating their telehealth billing policies; staying informed is critical.
- Understanding Place of Service Codes: Correctly identifying the place of service is essential for accurate reimbursement.
- Coding for Different Modalities: Different requirements may apply depending on whether services are delivered via audio-only calls or video consultations.
Impact: The complexity surrounding telehealth billing may lead to increased claim denials if services are not coded accurately, highlighting the need for specialized training in this area.
How QZ Medx Can Help: Our expertise in RCM encompasses all aspects of telehealth billing, ensuring clean claim submissions while helping you double your patient count and collections.
6. Emphasis on Clean Claim Submission
Submitting clean claims—those free from errors—is more crucial than ever in securing timely reimbursements from payers.
What to Expect:
- Increased Use of Claim Scrubbing Software: These tools help identify errors before claims submission.
- Focus on Documentation Accuracy: Thorough documentation supports the codes submitted on claims.
- Ongoing Training for Staff: Keeping billing teams updated on payer requirements is vital for minimizing errors.
Impact: A focus on clean claims will lead to reduced denials, faster reimbursements, and improved revenue cycle performance overall.
How QZ Medx Can Help: With an outstanding 98% claim acceptance rate, we help ensure minimal denials while maximizing revenue for your practice. Contact us today for a free consultation!
Staying Ahead of the Curve
The medical billing and coding landscape is dynamic, with numerous trends shaping its future. By staying informed about these key developments and partnering with a trusted RCM provider like QZ Medx, your practice can thrive well into 2025 and beyond. Don’t hesitate—schedule a free consultation with one of our experts today! Together, we can discuss your specific needs and demonstrate how QZ Medx can help you optimize your revenue cycle while empowering you to achieve your practice’s full potential.




